CPER Digest - December 2016
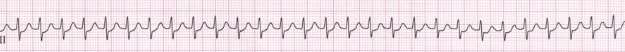
You and your partner are called for a patient complaining of a “racing heart”. Upon your arrival you find a 38 year old female patient sitting on her living room floor leaning against a couch. The patient is alert and oriented and appears to be in moderate distress. The patient tells you that she had a sudden onset of “racing heart” while at rest. She has experienced this before. She denies any chest pain or discomfort. She has associated complaints of weakness and dizziness when she attempts to stand. Together you and your partner begin to assess the patient while gathering a more detailed history. The patient states that she has a history of tachycardia/palpitations for which she takes diltiazem. She states that she has no allergies. You complete a set of vitals which are as follows: HR 180bpm, weak and regular, RR 18/min, regular and full with no adventitious sounds, SPO2 98% on room air, BP 124/60. Together, you and your partner examine the Lead II ECG strip below.
You initiate an IV while your partner acquires the 12 lead ECG below.
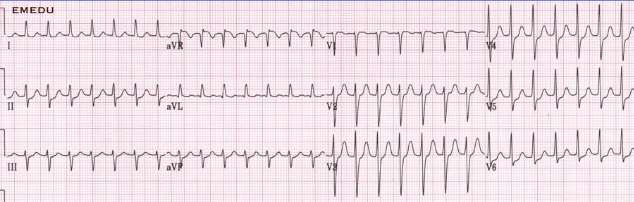
You both agree that the rhythm is fast and regular as you have mapped out the QRS complexes and the RR interval is the same rate and matches the cardiac monitor rate. You count out the number of small boxes (0.04 secs/small square) from the Q to the S and confirm the value from the 12 lead ECG printouts to be narrow (<0.12 secs). You note that there are no discernible P-waves. You presume this rhythm to be paroxysmal supraventricular tachycardia (PSVT).
Given that your patient meets the indications and conditions under the ACP Tachydysrhythmia Medical Directive (Cardiac section, page 87), what would be your next treatmentconsideration? If you said perform the Modified Valsalva manoeuvre that you learned at CPER’s Spring CME, you are correct! You explain the technique to your partner and to thepatient.
Within 60 seconds of performing the first of two possible attempts of the Modified Valsalva manoeuvre, the patient’s rhythm reverts to a sinus tachycardia at 114bpm and you ready the patient for transport. If the Modified Valsalva manoeuvre had not converted the rhythm from SVT to a sinus rhythm then BHP contact should be made for further treatment options (ie. adenosine or synchronized cardioversion).
The Modified Valsalva manoeuvre can be viewed at the following link https://www.youtube.com/watch?v=8DIRiOA_OsA. Evidence related to the effectiveness of this technique can be found at https://www.ncbi.nlm.nih.gov/pubmed/26314489.